Home Visits for the Unseen Five Percent: A Critical Priority for Closing Care Gaps

All payers and risk-bearing providers are familiar with the 80/20 rule of healthcare costs—the fact that approximately 20% of the Medicare patient population drive 80% of costs. However, as cost and reimbursement pressures on risk models increase, it’s becoming ever more critical to take a fresh look at additional opportunities to identify and better serve key populations. Meet ‘the unseen five percent’ – patients whose in-home assessment was the only documented source of care in the past 12 months – a population whose limited engagement has outsized implications for quality, outcomes, and member experience.
Who are the unseen five percent? And what contributes to their disconnection from the healthcare system?
In data analysis from one national health plan client’s Medicare Advantage membership1, Matrix Medical Network observed that about five percent of the members evaluated had gone 12 months or more without another source of care. These patients are effectively invisible to the healthcare system; they often have completely manageable medical issues that are highly risky for escalating into costly ED visits and avoidable inpatient admissions.
Claims data rarely tell the story of why a patient declined a screening or stopped seeing a primary care physician. The root causes are frequently social and logistical: transportation barriers, cost concerns, health literacy, fear of procedures, time off work or caregiving responsibilities. Online reviews and national surveys have consistently linked patient transportation issues to missed care appointments and later, downstream adverse outcomes. Interventions such as non-emergency medical transportation reduce patient no-shows even if long-term cost evidence is still evolving. In colorectal screening specifically, fear, lack of awareness, and logistics show up repeatedly in the literature as common barriers to participation.
“At Matrix Medical Network, we see firsthand how easily patients can slip through the cracks of the healthcare system—not because of a lack of need, but because of barriers that claims data can’t capture. A patient who misses a screening or avoids the doctor for a year often isn’t disengaged; they’re overwhelmed by challenges like transportation, cost or fear. These barriers are preventable, and when we address them head on, we not only reduce costly emergency visits and hospitalizations, we restore patients’ access to the care they deserve,” says Jeanette Richards, Senior Director of Clinical Excellence at Matrix Medical Network.
Closing care gaps among the five percent: The importance of the Comprehensive Health Assessment (CHA)
Industry evidence and field experience suggest that home-based comprehensive health assessments (CHAs) can be among the most effective tools for re-engaging disconnected members and addressing both clinical and social barriers to care.
A CHA model helps address common barriers directly at the source. In the home, clinicians can assess the physical environment, identifying fall hazards, food access problems, medication adherence and evidence of social isolation. For example, a clinician may discover that although a member reports they have “access” to food, their kitchen cupboards are nearly empty and the refrigerator light is off — a visibility that claims data or office-based visits would rarely capture. It also creates an in-person opportunity to clarify benefits, for example in transportation, mail-order labs or OTC allowances. Perhaps most importantly, it reconnects members to the healthcare ecosystem—translating data into direct action and follow-up. These visits also often surface previously undiagnosed or unmanaged chronic conditions—offering a path to earlier intervention before small issues become major costs.
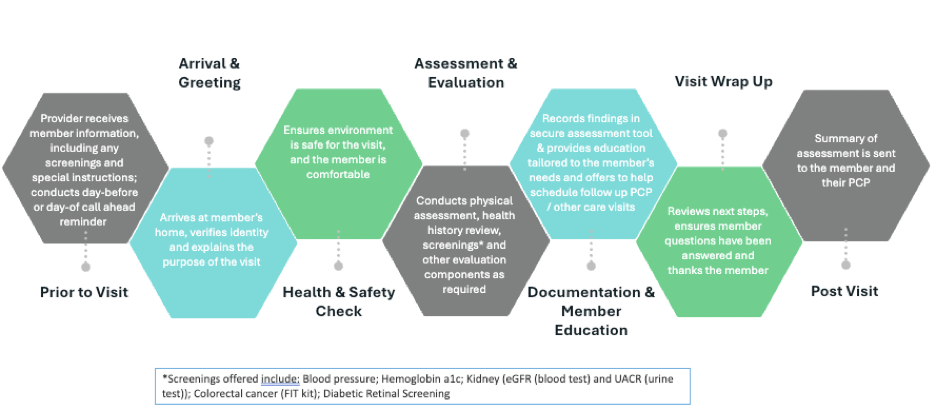
The CHA is a structured clinical encounter that brings evidence-based screening, a physical exam, targeted diagnostics, and benefit navigation into the patient’s living room—and then links those findings to timely follow-up care.
CHAs can reveal major opportunities for closing care gaps. Including:
- Identifying missed chronic conditions. E.g., hypertension, diabetes, chronic kidney disease
- Completing preventive tasks that count toward closing gaps in care. E.g., blood pressure capture, Fecal Immunochemical Test (FIT) kit completion, diabetic retinal exams, kidney health testing.
- Coordinating integrated downstream care in real time. For instance, by helping patients make a follow-up appointment with their primary care provider.
How the CHA model operationalizes these insights
Turning insight into impact requires consistent processes, data-driven prioritization, and coordinated follow-through. The first step is to stratify claims data for patients who are overdue for screenings or have rising-risk indicators (e.g., diabetes without recent uACR/eGFR, hypertension without a current blood pressure, diabetes without a retinal exam). CHA clinical education and coaching are designed to lower declination rates and improve clinical test follow-through.
During a patient’s CHA, clinicians will complete a focused patient history and exam; capture vitals; review and reconcile medications; facilitate on-site or near-site diagnostics; and document social needs that affect adherence to prescribed treatments and care plans. Crucially, the visit can operationalize care gap closure by ensuring follow-through on screenings and labs, not just offering them. This includes:
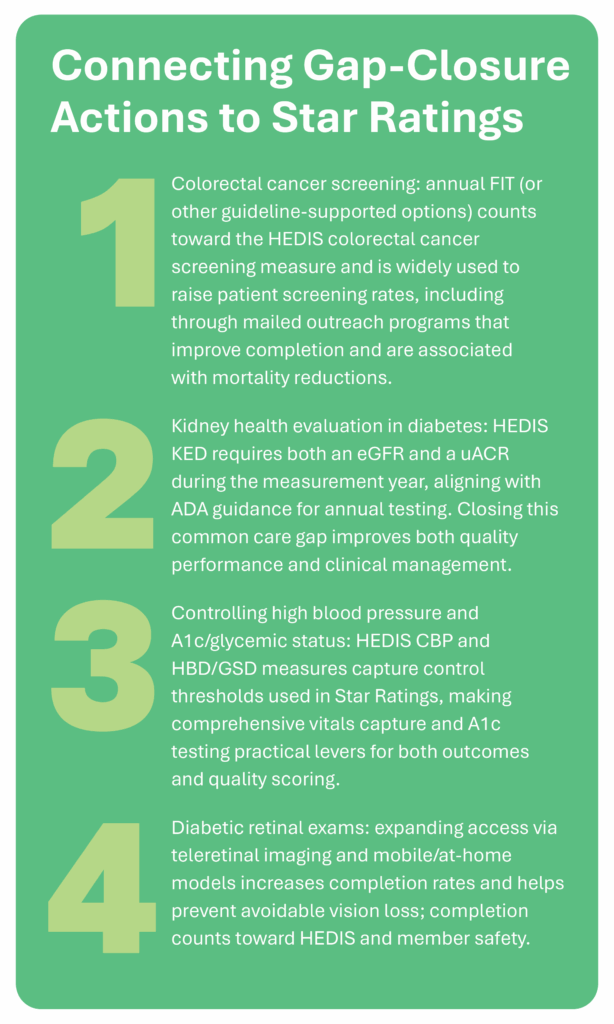
- Patient drop-off with instructions for FIT kits, which directly increase colorectal cancer screening completion rates with the potential to detect cancer sooner.
- Point-of-care A1c testing, enabling real-time identification of patients with uncontrolled diabetes.
- On-site or scheduled retinal exams via tele-retinal imaging partners, which help detect diabetic retinopathy earlier and boost exam completion.
- Standing lab orders for eGFR and uACR per ADA-aligned HEDIS® measure KED guidance — and, beyond standing orders, these tests can be conveniently performed in the home, reducing barriers to completion and improving monitoring of kidney disease progression in diabetic patients.
- Clinician-to-clinician escalation during CHAs when risk indicators are present.
After the visit, CHAs can serve as a bridge back to the system. Patient touch points and clinician referrals can be re-established in real-time; primary or specialty appointments are scheduled; and documentation is mapped to quality measure logic so that improvements are recognized in HEDIS and Star Ratings.
Benefits of closing care gaps via the CHA model
The benefits of closing care gaps using CHAs accrue both to patients, families and the organizations that care for them (payers and providers).
- On the patient side, evidence suggests that bringing screening into the home improves outcomes. It increases patient uptake of care and can reduce overall mortality for certain conditions2. Mailed FIT outreach and navigation programs systematically raise colorectal screening rates. Randomized and pragmatic clinical trials in community clinics and FQHCs show significant improvements in participation compared with usual care, and cohort evidence links FIT screening to lower colorectal cancer mortality. For example, a large U.S. nested case-control study of 10,711 individuals found that completing at least one fecal immunochemical test (FIT) was associated with a ~33% lower risk of dying from colorectal cancer (95% CI not reported for all groups).
A CHA model can also improve the patient experience by making care easier, safer and more understandable at home.
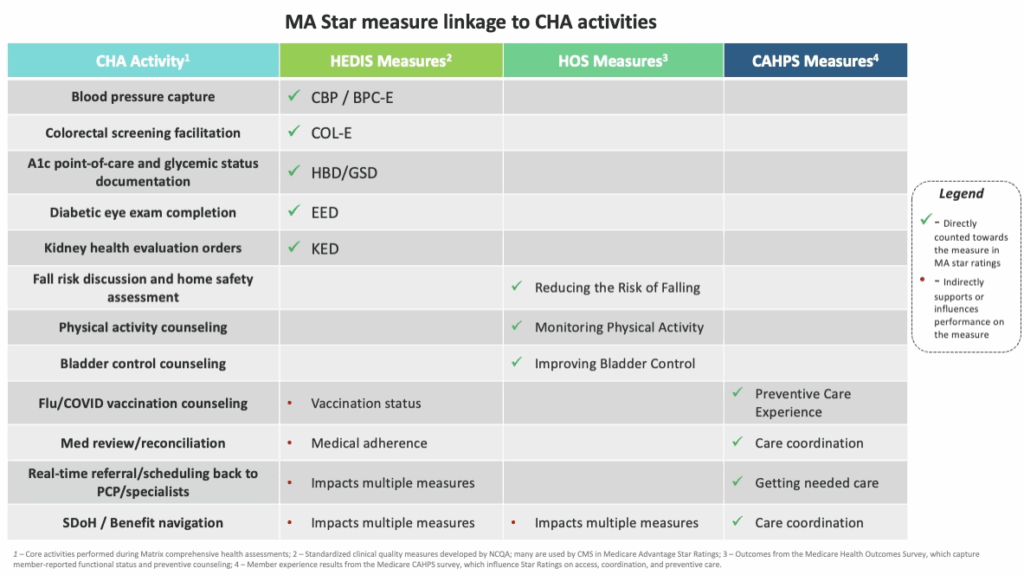
- On the strategic side for risk-bearing organizations, these care-gap-closing actions also align with widely used HEDIS measures such as rates of colorectal cancer screening, controlling high blood pressure, hemoglobin A1c/glycemic status, and kidney health evaluation for patients with diabetes—all of which CMS uses within the MA Star Ratings framework. This type of intervention also addresses drivers of patient-reported experience and function (HCAHPS/HOS) which, again, are crucial to payer and provider performance frameworks.
Conclusion
If roughly five percent of patients are invisible to the system, the costs will extend well beyond missed screenings. Every patient who feels disconnected from their providers and health plan is one step closer to attrition in a competitive Medicare Advantage marketplace. Every undiagnosed condition is a potential future readmission waiting to happen. Every delayed test is a gap in care that drags down Star Ratings and erodes the bonus payments that fund enhanced benefits.
Comprehensive, home-based assessments make invisible members visible again—connecting evidence-based screening with real-time follow-through, and turning intent into action. We believe the home is where that transformation begins.
For organizations seeking to strengthen quality performance and member trust, the path often starts with seeing—and serving—the unseen five percent.

- Finding based on Matrix Medical Network analysis of Medicare Advantage members from one national health plan client; see [Matrix Medical Network Whitepaper on Closing Gaps in Care] for details. Available to prospective clients upon request ↩︎
- “Fecal Immunochemical Test Screening and Risk of Colorectal Cancer Death” (2024): nested case-control across large U.S. health systems; FIT completion was associated with ~33% lower CRC mortality ↩︎
Related Posts
Protecting the Human Side of Data: A Pragmatic Approach to Patient Privacy
Maintaining the security of digital health records has evolved from an IT requirement into a core pillar of patient trust and operational stability. For risk-bearing organizations, a single data vulnerability does more than trigger regulatory penalties; it disrupts the continuity of care and impacts the provider-patient relationship. As your network…
How 2026’s Health Tech Trends are Humanizing the Patient Journey
The year 2026 represents a definitive point in the digital transformation of global healthcare. For nearly a decade, the industry focused on the foundational task of converting paper records into digital bits. However, as we enter 2026, the strategic priority has shifted toward how remote patient monitoring is utilized to…
Caring Through the Holidays: Special Considerations and Safety Tips for Seniors Receiving In-Home Care
For many people, the holiday season is a time of celebration and connection. For seniors and homebound individuals, however, this time of year can introduce added risks and challenges that impact both physical and emotional well-being. Changes in routine, colder weather and increased social isolation can all influence health outcomes,…